The gut-immune-brain connection:
Over 70% of your immune system is located in your gut!
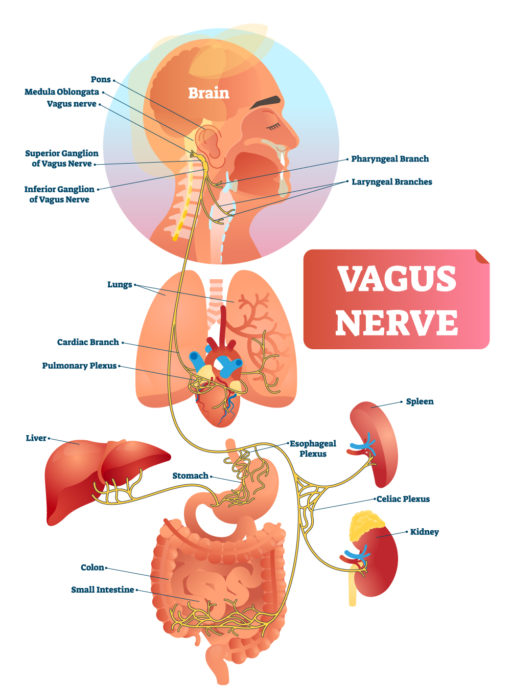
Two thin layers of more than 500 million nerve cells line your gastrointestinal tract from esophagus to rectum—the enteric nervous system (ENS). These sensory nerves in turn communicate gut status to one of the largest and most complex nerves in the body, the vagus nerve. Nearly 90% of the fibers in the vagus nerve transmit signals TO the brain from the rest of the body that regulate your heart rate, breathing, and is THE way that your gut talks to the 100 billion nerve cells in the brain. This is the gut-immune-brain connection.
The trillions of microbes that live in your gut if they are the right beneficial strains, make chemicals that affect how your brain works and communicate the status of health to the brain. An incorrect balance of microbes (not enough beneficial or health promoting and too many pathogenic—or even commensal, meaning neither helpful nor hurtful) destroy the gut wall’s integrity and communicate this state of inflammation to the brain via both electrical nerves and a different set of hormones.
Your gut releases hormones into the bloodstream to communicate hunger, satiety, inflammation, infection, and more… electrical nervous signals are fast as lightning while hormones are slow. A healthy blood brain barrier and a healthy brain are there due to that state of good health. A broken, “leaky” blood brain barrier and an inflamed brain is associated with disease. Worse, if there has been any sort of trauma to the brain, whether from injury, stress, too many drugs or alcohol, as well as the fact of these inflammatory electrical and hormonal signals, it will heal only slowly, if at all. Until gut integrity is also corrected, symptoms persist.
Diseases known to result from lost gut-immune-brain integrity:
A number
of debilitating diseases require having digestive inflammation or “leaky gut” including Autism Spectrum Disorder, Autoimmune diseases. Stroke, and “Psychiatric” conditions (easily remedied by restoring gut health). Another set of diseases thought to be caused by “leaky brain” include Siezures, Multiple Sclerosis, Alzheimers, Declining muscle coordination (and therefore tone), others…
Taken together, these facts highlight the importance of keeping your digestive tract healthy—which will keep you emotionally and physically healthy, too!
Keys to a healthy gut
Maintain a correctly balanced gut microbiome (the collection of microbes, bacteria, viruses, protozoa, and fungi/yeast naturally living in the gut. A balanced microbiome:
- creates immune balance—not too much (autoimmune), not too little (“catch” everything and cancer),
- prevents disease, a balanced microbiome is more powerful than antibiotics (which will destroy it),
- supports emotional well-being by creating electrical nerve stimulation and hormones that signal health,
- helps remove toxic waste,
- helps digest food,
- directly activates or deactivates and balance certain hormones such as thyroid and cortisol
- reduces allergies.
Keeping your gut microbes happy and flourishing will help them help you!
How the inflamed gut breaks down the blood brain barrier or prevents healing.
Which bacteria live in you (among yeast, viruses, protozoa etc.) determine what gets produced when they ferment fibers. If the foods you eat produce gas that cause bloating or any inflammatory reaction (hives, eczema, joint pain…), your immune system knows there is an unhealthy microbiome. In turn, the immune system tells this to the brain and/or directly breaks down the blood/brain barrier and inflames the brain. It works like this:
- Your immune system is responding to the disturbed microbiome (which has inflamed the gut causing “leaks”).
- All the components of the microbiome as well as incompletely processed food and even waste products leak out through these gaps.
- This further activates your immune system.
- The immune system fights these invaders by releasing chemical warfare (cytokines) into the area. These chemicals also go into the blood and are part of what contribute to degrading the blood brain barrier.
Helpful bacteria live on plant fibers in the presence of adequate stomach acid.
Prebiotics: feeds a healthy microbiome so it remains pro health. These are typically fibers that are fermented by your gut bacteria. Fibers come from plants and seeds including beans (legumes). Chia and Flax seeds are especially useful as they are a good source of omega-3 fats, some protein, and will help keep you regular. There are also some good commercial fibers like Standard Process’ Whole Food Fiber and Prosynbiotic which is a combination of both prebiotic fiber and probiotics.
Proper digestion of these fibers starts with adequate stomach acid production. The bottom line: Before jumping to stomach acid inhibitors (which prevent release and absorption of B12 and iron from animal and fish, and many minerals as well) consider which food choices are causing the reflux, (commonly dairy, cereal grains, commercial fats, sometimes alcohol, caffeine… large meals…). These inflammatory foods or improperly digested foods/fibers cause small intestine bloating or colon gas. It can also cause colon bacteria to move into the small intestine, another form of microbiome disturbance.
- Remove inflammatory foods: Work with me on understanding and eliminating irritant foods while improving stomach and digestive enzyme function, usually with supplements in this step. Also ensure healthy liver and pancreas function. If these organs are not producing adequate bile and digestive enzymes, you will not digest your food or absorb nutrients properly. Nutrient malabsorption has important health implications including higher risk of bone fractures, more fatigue, and immune imbalances.
- Replace with nutrient dense foods: Work with me to determine which foods to add back in first both to support your nutritional needs and heal what your body says is a priority. That said, it’s vital to keep your additions simple. Adding many foods at once could trigger an inflammatory response that will be impossible to understand with so many new things. Production of digestive enzymes declines with age and most of us need support to get the most out of our food.
- Reinocculate: This is most successful when you shift your food choices to feed and support the microbes you want while starving those you don’t. Sugar, processed foods, and cereal grains support an unhealthy microbiome. Plants and grass-fed or wild caught animal products (avoid grain finished and anything that has been given antibiotics or hormones). Probiotic supplements serve their purpose to aid in digestion and antibiotic functions; however, they do not “take over” an unhealthy microbiome.
- Repair: See next sections…
Raise the alarm!
The public will demand [the antibiotic and] … then will begin an era … of abuses and the evolution of resistance.
My son is sleeping!
For the first time in four years our son is sleeping through the night. This is HUGE. I’m no longer getting “pick him up now” calls from day care because he’s misbehaving. I’m beginning to lead a normal life. Thank you, Marie, for being so caring and patient. I know it was all from his digestive issues and you are our personal hero for helping us solve them. There is nothing better than seeing our son begin to enjoy his life.
Sleepless in Alaska
I started my Nutrition Response Testing program because I was very tired, couldn’t sleep—I actually felt ‘wired’ at night—and I was profoundly unmotivated. Now I’ve lost weight, sleep through the night, and have much better energy. Because of this, I’m back to being really active and have a dramatically more positive attitude.
Balance your gut microbes, heal your gut, and improve immunity. Heal your brain.
Bio-individuality: You are unique. It is vital to assess whether a particular set of foods or health practice is appropriate for your unique body. Just because something sounds good or seems like it should be healthy doesn’t mean it’s realistic, or even safe, to apply to your own life. Consider this: Humans share 99% of the same genetics, yet 10% or less of the same microbiome! Not all guts (or other organs) are created equally. Not all bodies respond equally!
Second, and this is very important! Just like a “New Year’s Resolution” you might initially be motivated to dive “all in”. But change is most attainable and long-lasting with small sustainable shifts. Shifting your gut health does not take long and it will result in a far improved gut-immune-brain connection.
Pick ONE suggestion that you can truly do, get comfortable with that new routine, then pick another… and so on.
Improve your gut health to improve your immunity:
 Eat a rainbow of plant-based foods.
Eat a rainbow of plant-based foods.
Colorful fruits and vegetables look beautiful on your plate. Beautiful food tells family and friends you took care to make something wonderful. And it creates interest in eating these foods.
This can be quick! The more inflammatory foods you eliminate, the faster you feel well. Then work with me to decide what to add back in, and in what order, there is a method.
Nutritionally, colorful plants are important for getting diverse sources of fiber, vitamins, antioxidants, and minerals. Plant fibers set the stage for diverse microbial populations in the gut. When diets lack fiber (plant tops and roots, beans, nuts) beneficial bacteria are lost, and their health benefits are lost. Consume sugars and processed foods and the microbiome is disrupted.
How to incorporate colorful foods into your diet:
- Download the Rainbow Foods for Organs Handout. Read the specific foods to help your priority organ on page 2.
- Take a baseline assessment of how many servings (fist-sized portions) of fruits and vegetables you’re eating in a day. Track it for one week to get an average. Set goals to gradually increase the average number of fruits and vegetables you eat daily (bonus points if you track the number of colors eaten, too!).
- Choose two colored vegetables for at least one meal. Ideas: sauté green and orange peppers for a stir-fry; chop up yellow summer squash and red tomatoes for a salad (bonus points for including greens.
- Make a grocery list for shopping where you write down the produce you plan to purchase by color. What simple recipe swaps can you make to include a rainbow of foods?
Make bone broth soups with plenty of cooked vegetables.
Bone broth is naturally healing and both gut and brain balancing providing the cells of your digestive lining with a great source of protein, minerals, and antioxidants. Grab my recipe here. Use it as a base for soups with your rainbow of vegetables like Energy Soup: Carrot Apple & Ginger, Moroccan Pureed Yam Soup, Rejuvenating Chicken Asparagus Soup... among some favorites.
Pump up the probiotic foods:
Choose probiotic foods, not supplements, unless specific to your Nutrition Response Testing plan.
We all have microorganisms in our gut, our mouth, on our skin, in our lungs… that provide health benefits. Having the right types is key to good organ, skin, gut, and brain health as well as a robust immune system.
For your brain: Probiotics (the right ones in the right places) produce short-chain fatty acids (SCFAs), such as butyrate. These play a role in regulating the immune system, they feed your energy hungry liver, and brain to maintain brain health.
Every strain has a different benefit. Look at it this way: Dogs are all canines. Among dogs there are chihuahuas, poodles, great Danes, Siberian huskeys… Some of us love lap dogs; others love dogs who run with the wind. It’s all good. Probiotics have strains, dogs have breeds.
Even if it boasts a high strain count (and many don’t or need refrigeration), consider that the strains in supplements may not be the “breed” you want for your situation. I use Probiotic Advisor (a searchable database that evaluates commercial products against scientific evidence) and Nutrition Response Testing can work out the best solution.
How to incorporate probiotics into your diet:
 Make coconut milk kefir and use in smoothies, creamy buckwheat cereal, or in chia pudding.
Make coconut milk kefir and use in smoothies, creamy buckwheat cereal, or in chia pudding.
Make fermented vegetables, (or buy some: Bubba’s sauerkraut or Wild Brine beet slaw. These are great and available at Fred Meyers). There are many recipes on OurNutritionKitchen.com or download the handout to add to your recipe collection. If you do, please vary them and please check in with your bio-individuality! Incorporate them slowly—a few tablespoons at a time—and if you already have gastrointestinal issues, especially SIBO, IBS, or IBD, discuss the use of supplements and probiotic foods with me first. Not everyone tolerates probiotic-rich foods (hello, bloating!), and they’re actually not recommended at all if you experience immunosuppression or have a histamine intolerance.
Make naturally fermented pickles instead of vinegar pickles to add to tuna salad or on burgers (or even hot dogs because you can buy sugar and nitrate free meats here).
Continue to pile on the prebiotics.
What’s a prebiotic? These are nondigestible (by us) plant fibers that “feed” the microbiome (the healthy balance of bacteria, virus, yeast…) that you want living in your gut.
Your gut is like a garden; probiotics are the flowers, herbs, berry bushes, and trees; prebiotics are the healthy soil with organic nutrients that help them grow.
This, and only this, is how you can improve the balance of probiotics in your gut. Taking probiotic supplements (the right ones) can be extraordinarily therapeutic but it doesn’t change your microbiome from an unhealthy mix to a healthy one. Only your dietary choice along with removing toxic chemicals, metals, any parasites… can do that. Why would you want to do that?
- boosts immunity,
- prevents disease,
- supports emotional well-being,
- helps remove toxic waste,
- helps digest food,
- directly activates and balances certain hormones.
Just like probiotics, prebiotic supplements may or may not be right for you and certain foods may cause bloating and other discomforts. If you already have gastrointestinal issues, start with well-cooked vegetables, limit fruits, and avoid beans (for now). Once there is more balance, these can be added.
Prebiotic foods:
- Love tea? Sip on a cup of prebiotics: Chamomile, green, roiboos, chicory root or fennel teas are wonderful!
- Eat plant-based meals frequently. Pastured and wild meats are healthy—still, most of us need more plants in our diet.
- Make a breakfast shake with berries, whey protein, unsweetened almond milk, and a Tablespoon or so of either chia or flax seeds. Check out other recipes at OurNutritionKitchen.com
Stress less.
Stress directly impacts gut microbes and leads to inflammation. Interestingly, it looks like constant stress changes your microbiome in several ways:
Stress reduces the amount of SCFAs needed for immune, brain, and other organ health.
If it goes on too long, chronic stress will alter the integrity of the intestinal barrier. Even if your diet is perfect, stress alone can lead to the breakdown of your intestinal lining, what we call. Leaky gut increases inflammation. It is also a factor in developing autoimmune diseases in predisposed individuals (autoimmune has a genetic component).
How to decrease stress for better gut health:
- Brainstorm a list of people, places, and activities that are comforting to you. Pick friends who won’t evaluate, invalidate, or otherwise analyze; its more therapeutic to take your mind off it all and simply enjoy another or other’s company doing something you love.
- Use this breathing technique: Take a full breath in for 8 seconds, feel your belly rise. Pause, holding your breath for 4 seconds. Open your mouth and exhale slowly for 8 seconds. Repeat as needed. This also lowers blood pressure.
- Go for a walk and look at pretty things! Nature is known for its mood-boosting benefits. Feel the sunshine on your skin for a minute or two. Even if it’s raining, just look. Find something and look at it, admire it.
 Play in the dirt.
Play in the dirt.
Get outside, go barefoot, walk on the beach or your yard.
There are nearly one billion beneficial microbes in one teaspoon of soil! Playing in the dirt modifies gut microbiota, leading to anti-inflammatory and immune-supporting benefits. Overly sanitized environments lower gut microbe diversity; it’s important to maintain diversity
Dirt aside, the prevalence of allergies is lower in individuals living in rural areas as they’ve developed an enhanced immune tolerance.
“Play in the dirt”:
- Visit a natural area a few times per week. Take a hike anywhere, many of us have favorite camping spots, cabins, Kincaid beach is super... After work, I often hike the Turnagain arm trail or Blueberry hill below Flat-top for a short outside activity.
- If you have more time, drive to the Wildlife Conservatory just past Girdwood. Their mission is to rehabilitate injured animals and even bring lost herds of bison back to Alaska.
- Grow a garden or plant a few potted plants.
Letting your skin play in dirt will change many things.
Trust your gut feelings
Take the concept of trusting your gut to the next level! When your gut tells you that something isn’t quite right, it can manifest as an emotion, such as fear, or a physical symptom, such as gastrointestinal distress. Listen to it.
And when you bring me your food and mood log, mark down how you are feeling. You'd be surprised!
I’ve lost 14 pounds
I wasn’t really looking for a weight loss program. I actually had a mysterious skin rash that wouldn’t go away. That cleared up fairly quickly and as I continued with my Nutrition Response Testing program I began to feel much more energy. I noticed my clothes started fitting differently; my friends and husband noticed too.
I’ve gotten so much more than I expected. Thank you Marie!
My body can heal itself
Marie has taught me that if I don’t avoid the things that cause damage (certain – foods, topical products, vitamins…) , over time it can cause problems. Good foods build our health and can heal us.
Inflammation, good vs bad
The body can heal itself with the right tools. Some inflammation is okay, but having it long term is not good. It’s important to pay attention to what causes inflammation.
There is hope and I can help.
Call me 907-222-1824
Desai, M.S., Seekatz, A.M, Koropatkin,N.M, Kamada, N.Hickey, C.H, Wolter,M. … Martens, E.C. (2016) A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility. Cell 167, 1339–1353 November 17, 2016 2016 Elsevier Inc. http://dx.doi.org/10.1016/j.cell.2016.10.043
Frei, R., Akdis, M., & O'Mahony, L. (2015). Prebiotics, probiotics, synbiotics, and the immune system: experimental data and clinical evidence. Current opinion in gastroenterology, 31(2), 153–158.
Ito, T., & Jensen, R. T. (2010). Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium. Current gastroenterology reports, 12(6), 448–457. https://doi.org/10.1007/s11894-010-0141-0
Lach, G., Schellekens, H., Dinan, T. G., & Cryan, J. F. (2018). Anxiety, Depression, and the Microbiome: A Role for Gut Peptides. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics, 15(1), 36–59. https://doi.org/10.1007/s13311-017-0585-0
Lloyd-Price, J., Abu-Ali, G., & Huttenhower, C. (2016). The healthy human microbiome. Genome medicine, 8(1), 51. https://doi.org/10.1186/s13073-016-0307-y
Pasolli, E., Asnicar, F., Manara, S., Zolfo, M., Karcher, N., Armanini, F., Beghini, F., Manghi, P., Tett, A., Ghensi, P., Collado, M. C., Rice, B. L., DuLong, C., Morgan, X. C., Golden, C. D., Quince, C., Huttenhower, C., & Segata, N. (2019). Extensive Unexplored Human Microbiome Diversity Revealed by Over 150,000 Genomes from Metagenomes Spanning Age, Geography, and Lifestyle. Cell, 176(3), 649–662.e20. https://doi.org/10.1016/j.cell.2019.01.001
Maltz, R. M., Keirsey, J., Kim, S. C., Mackos, A. R., Gharaibeh, R. Z., Moore, C. C., Xu, J., Somogyi, A., & Bailey, M. T. (2019). Social Stress Affects Colonic Inflammation, the Gut Microbiome, and Short-chain Fatty Acid Levels and Receptors. Journal of pediatric gastroenterology and nutrition, 68(4), 533–540. https://doi.org/10.1097/MPG.0000000000002226
Morris, G., Fernandes, B. S., Puri, B. K., Walker, A. J., Carvalho, A. F., & Berk, M. (2018). Leaky brain in neurological and psychiatric disorders: Drivers and consequences. The Australian and New Zealand journal of psychiatry, 52(10), 924–948
Sonnenburg, E. D., Smits, S. A., Tikhonov, M., Higginbottom, S. K., Wingreen, N. S., & Sonnenburg, J. L. (2016). Diet-induced extinctions in the gut microbiota compound over generations. Nature, 529(7585), 212–215
Tasnim, N., Abulizi, N., Pither, J., Hart, M. M., & Gibson, D. L. (2017). Linking the Gut Microbial Ecosystem with the Environment: Does Gut Health Depend on Where We Live?. Frontiers in microbiology, 8, 1935. https://doi.org/10.3389/fmicb.2017.01935
Volta, U., Bardella, M. T., Calabrò, A., Troncone, R., Corazza, G. R., & Study Group for Non-Celiac Gluten Sensitivity (2014). An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC medicine, 12, 85. https://doi.org/10.1186/1741-7015-12-85


Leave a Reply
You must be logged in to post a comment.