There’s very exciting news to share for those with autoimmune situations like Inflammatory Bowel Disease (IBD). The Paleo autoimmune protocol (AIP) has been put to the test in a formal research study, and the results are fantastic.
It’s incredibly hard to get a nutritional study funded. Pharmaceutical companies don’t profit. If there is only on anecdotal or observational evidence (case reports, etc.) this overturns current paradigms in clinical research. No agency wants to fund something that is “too out there” or “doesn’t yet have any evidence.”
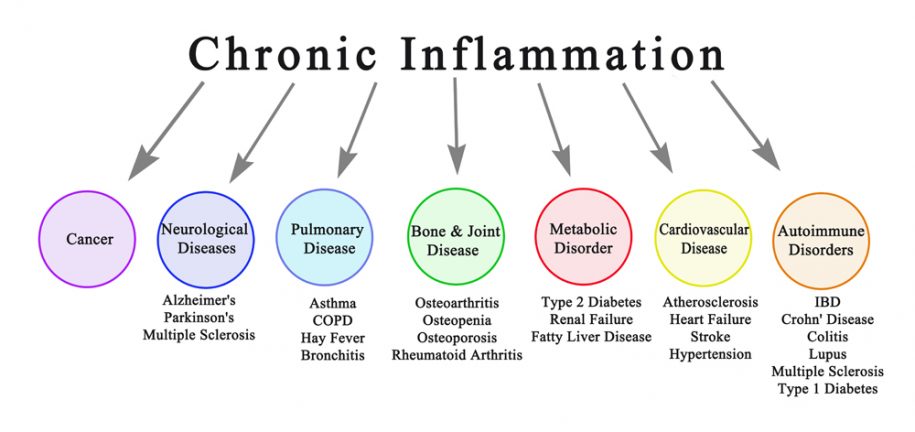
What do we know? Autoimmune diseases occur when the body begins to attack itself. Why? Three things align in a perfect storm:
- Genetic predisposition (as of 2015 some 231 genetic variants increase IBD risk alone).
- Gut imbalances (breakdown of the digestive tract protective layers, microbial imbalances e.g. SIBO/SIFO/SIMO, Irritable Bowel Syndrome (IBS), etc.)
- A trigger (chemical exposure, infection, smoking, food irritants, stress…)
You are not your genes; there must be a trigger
Genetics only accounts for a very small portion of how autoimmune disease manifests: 8.2 percent increased risk for Crohn’s disease and 13.1 percent for ulcerative colitis.
Some 65 percent of people with IBD have known food sensitivities and most do not know (or don’t want to believe) which foods are irritating them. This is also true for other forms of autoimmune like SjÖgrens, Hashimoto, Grave, Diabetes… however those flare-ups often take weeks after ingesting the offending food while gastrointestinal distress is more easily linked to foods. IBD affects some 1.5 million people in the United States.
Importantly, food sensitivity and allergy testing is extremely imprecise. Too many of my clients have long lists of food and environmental allergens they are told to avoid. When we do a standard elimination diet and then monitor reintroductions intelligently, most of my clients find they can tolerate foods that tested positive as allergens.
Because medications that suppress the immune system have unwanted other effects including being susceptible to viruses, bacteria, even cancer, nutritional therapy is a key step in addressing the wide range of IBD symptoms including GI pain, bleeding, bloating, fatigue, and malnourishment.
[testimonial_category=”autoimmune”]
What is the Paleo Autoimmune Protocol (AIP)
Certain foods are inflammatory to most: cereal grains, dairy, refined seed oils, cane and corn sugar. Paleo protocols also remove legumes (beans) and the Paleo autoimmune protocol recommends removing eggs, nightshades (potatoes, tomatoes, eggplant, peppers), coffee, alcohol, nuts, and seeds. These restrictions are aimed at healing and sealing the digestive tract by avoiding foods that trigger intestinal inflammation or intestinal microbial imbalances.
Like Paleo, AIP emphasizes nutrient-dense, healing foods in all phases:
- The initial elimination phase emphaizes bone broths, fermented foods, and steamed veggies
- The protocol next transitions to a maintenance phase to stabilize symptoms.
- Finally, the protocol transitions to a structured reintroduction phase where select foods or food groups are carefully returned to the diet and monitored for any signs of irritation.
Study #1 Standard American Diet (SAD) to AIP in 6 weeks
Fifteen patients living with IBD for, on average, 19 years, transitioned from their current diet (SAD, although some had eliminated obvious irritants) to AIP over 6 weeks. They then remained on the AIP restrictive diet for an additional 5 weeks. Individuals who tested for vitamin D or iron deficiency (common in IBS) were provided supplements. Half the individuals were actively taking immune suppressing medications at the start of the protocol.
By week six, 11 of the 15 participants (73%) achieved clinical remission as measured by inlamaatory markers (fecal calprotectin) and lesions via colonoscopy. Four of the seven on medications were able to discontinue those completely. Nor more side effects. Three of the 15 elected to discontinue the elimination diet phase after 6 weeks.
Study #2 AIP Returns Quality of Life in 3 weeks
The same 15 individuals with Ulcerative Colitis (n=6) or Crohns Disease (n=9) were asked to complete questionnaires every three weeks to describe their quality of life based on questions about their activity levels and social interactions.
Within the first three weeks, quality of life increased by 20%, at nearly three months (week 11), the improvement had stabilized. Individuals reported doing more of what they want to do without the limitations of IBD.
Study #3 The Specific Carbohydrate Diet (SCD)
Taking a slightly different approach, this strategy eliminates grains, dairy, and refined sugars. In just two months, 2-3 months, nearly a third of clients were symptom free, however markers of inflammation and colon lesions were not monitored.
The Bottom Line with IBD and Other Autoimmune disease
What do these protocols have in common?
My goal when I work with clients is to achieve the least restrictive and sustainable diet possible that provides the most amount of health, vitality, and life. It is easy to become fearful of adding foods back in. In fact, only a few people with autoimmune (or other immune stress) need to strictly and permanently avoid foods eliminated during the first week. That is what the reintroduction phase is aimed at understanding.
Once you take enough stress off the body and emphasize enough genuine building blocks, true healing begins.
Commit 100% to a Paleo Reset for 30 Days
Remove foods that could trigger inflammation or harm gut health while emphasizing nutrient-dense foods that promote health.
Optimize nutrient intake with foods that promote health
- Bone broth
- Liver
- Fermented foods
- High-quality meats from 100% pastured or wild animals and fish
- Leafy and cruciferous vegetables
- Healthy fats from whole plants and animals (avocado, olive, walnut, coconut, butter from pastured animals, ghee…)
Reduce the immune response using the general paleo template by removing foods like:
- Cereal grains (wheat, including heritage wheats; corn; rice; oats; barley; rye)
- Legumes
- Dairy
- Industrial seed oils
- Refined sugar (Cane—even organic turbinado is a nervous system toxin, Corn, Agave)
Remove the foods and toxins that contribute to the over-reactive autoimmune response will help reduce symptoms and put the disease into remission.
If the general paleo template isn’t enough, try the Paleo Autoimmune Protocol by removing:
- Eggs
- Nightshades (like eggplants, tomatoes, and potatoes)
- Coffee
- Alcohol
- Nuts
- Seeds
- Ensure all meat and fish are pastured (100% grass fed or wild)
Eat enough calories and reintroduce foods systematically
Reintroducing foods is perhaps the most challenging aspect. There are strategies for proper elimination and proper reintroduction to achieve an enjoyable and broader diet—both at home and when eating out. Some of my clients do well with nutrient-dense pasture-raised eggs after eliminating the cheap junk eggs for a while. Others do well with (infrequent) amounts of raw milk cheese (although, to date, none do well with milk).
Don’t rush reintroductions! Don’t be afraid either.
Choose which foods are the most important to you to try reintroducing, and then work systematically to bring them back into your diet. I rarely suggest trying to reintroduce gluten if you have an autoimmune disease, but other excluded foods like dairy, eggs, nightshades, and/or nuts and seeds, and even non-Paleo foods like Forbidden rice and legumes, can frequently be tolerated by those with an autoimmune disease. By systematic is meant one new food group at a time and at the first sign of symptoms remove that food again.
Would you like a sample meal plan? Click Here
For example, Ghee has the least milk proteins, then butter, then hard cheeses (because the bacteria works its miracles). Nightshades are nutrient dense (except Russet Potatoes), but each one is different and must be reintroduced one at a time. There is a strategy.
That said, if medications were needed for 19 years, wouldn’t it be worth trying a nutritional plan for 6 months?

Leave a Reply
You must be logged in to post a comment.