 The thought of eliminating hot flashes and feeling great might seem too good to be true. Annoying they are; there is no reason to be miserable through perimenopause, menopause, or even for years after.
The thought of eliminating hot flashes and feeling great might seem too good to be true. Annoying they are; there is no reason to be miserable through perimenopause, menopause, or even for years after.
What do hot flashes, fatigue, weight gain, and decreased sex drive all have in common? The changing hormones through the menopause transition; or in some cases the abrupt menopause following a hysterectomy. Certain breast cancer medications can also completely shut off normal hormone production by lowering estrogen.
By far, the biggest discomfort involves hot flashes and night sweats. While annoying, these will go away over time. After that, it’s vaginal dryness leading to potentially painful sex and decreased libido. Importantly, these do not go away over time but there are ways to manage it. Next up is insomnia—if being woken up by hot flashes and/or night sweats then taking steps to balance hormones may help. However, sleep disturbances naturally increase with age and in many cases raising estrogen or other hormones may not help. Mood changes, commonly anxiety and depression, may be secondary to sleep disturbances as is weight change. Waking up unrested contributes to daytime fatigue, issues at work or with friends and family, loss of motivation, and depression.
For decades estrogen has been added in tiny amounts to various “anti-wrinkle” creams. Ingredients under 5 percent of the total do not need to be listed on the label. The estrogen helps plump out the fat cells underneath the skin but repeated application can lead to waistline and other weight gain.
Add to the list of health concerns that increase as estrogen wanes: Risk of developing osteopenia and osteoporosis, increased risk of cardiovascular problems, poor concentration, poor memory and increased risk of dementia, hair thinning or loss, increased risk of urinary tract infections and/or incontinence, bloating and/or fluid retention, and hormone pattern acne.
With all that, you may be thinking about hormone replacement therapy (HRT). By understanding your options, you can make an informed choice. There are many steps to take before jumping to HRT.
First a primer on menopausal hormone change and health implications.
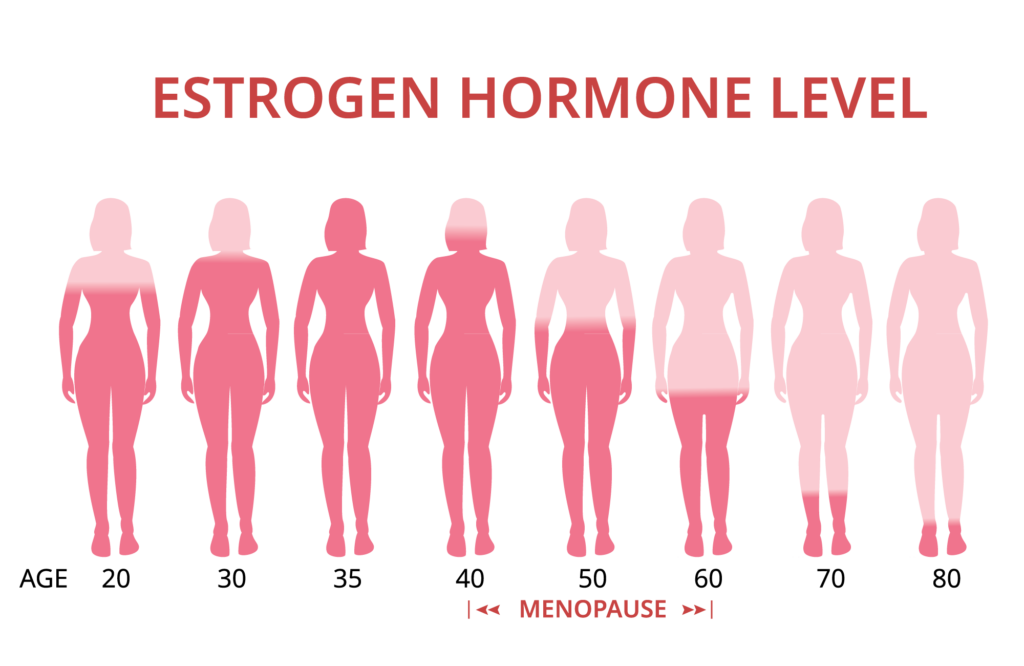
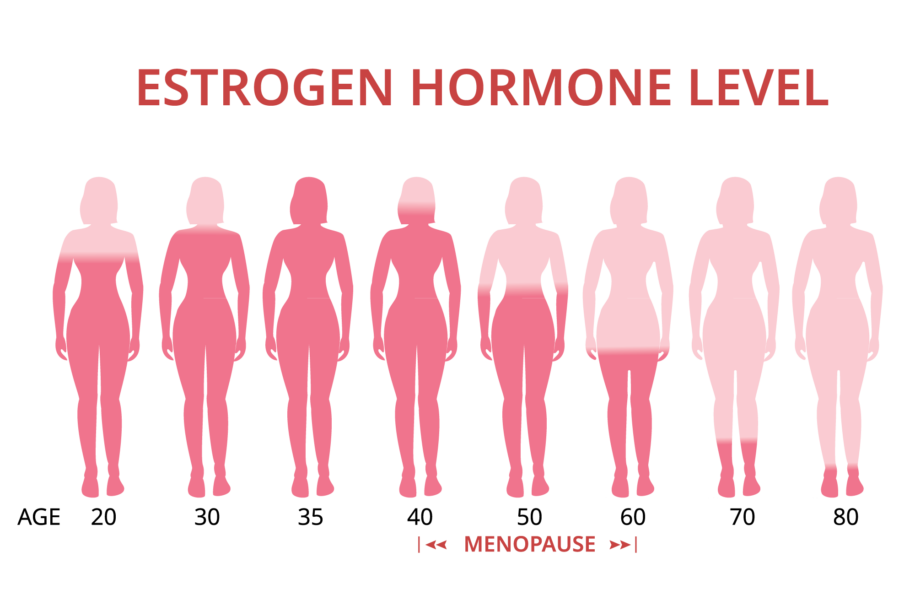
Natural menopause is a gradual transition from childbearing years. Called perimenopause (menstrual cycles become less regular), this transition can last nearly 15 years. The transition typically occurs between ages 45-60 but age can vary.
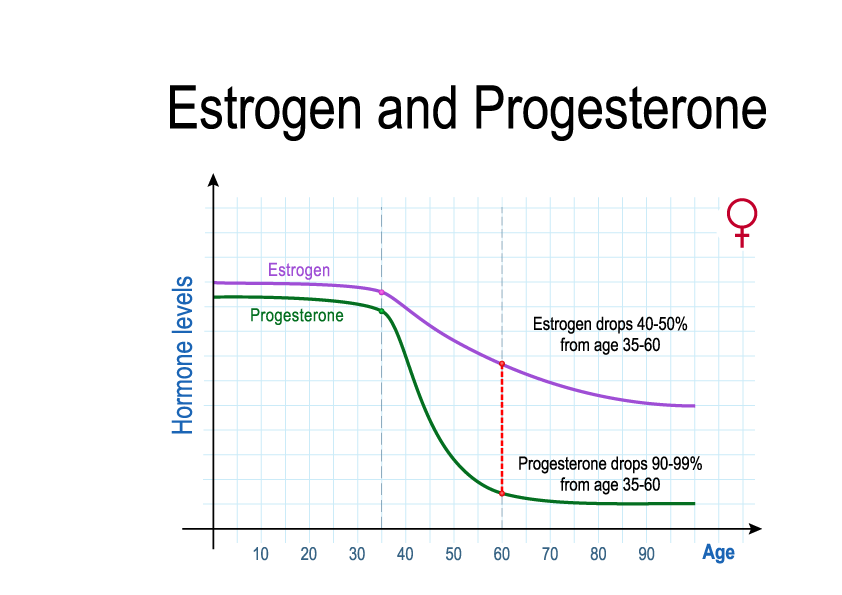
During child-bearing years, our ovaries make ten times more estrogen and progesterone; after menopause the ovaries make very little of either. Menopause is the gradual transition from ovarian estrogens (Mainly estradiol) to a main estrogen produced in the adrenal glands (mainly estrone). During child-bearing years, ovaries also make one-fourth of all of our testosterone—the rest is made largely in the adrenal glands but all cells of the body can make it from precursors made in the adrenal glands. Menopause also transitions testosterone manufacture to the adrenal glands.
Some 68-80 percent of women in the U.S. experience hot flashes; yet 60 percent in Sweden and Australia, only 40 percent in Italy. Heritage appears to make a difference with only 10-25 percent of Indonesian and Chinese women reporting symptoms and Latin American women none.
What’s different between these regions? Diet and how foods and animals are raised. Genetics applies to certain cultures but what stands out the most is Mediterranean vs. Regional vs. Western diet and lifestyle.
Something can be done about it.
Menopause created by surgically removing the uterus (sometimes with ovaries) is more abrupt. Only 10 percent of women escape having hot flashes.
What, exactly, is a hot flash?
Basically, a hot flash involves blood vessel dilation that elevates skin temperature causing sweating and flushing. This results in heat loss; followed by chills, clamminess, and anxiety. One-third of women who have hot flashes report more than 10 per day, generally lasting 1–5 minutes with about six percent lasting more than 6 minutes. Often, women can tell when a hot flash is about to start.
Who is more likely to experience hot flashes?
- Overweight women;
- Thin women who smoked during their premenopausal years have more hot flashes than non-smoking overweight women;
- Western women especially the U.S.;
- Consuming refined foods (especially late-night snacks) (especially sugary foods);
- Alcohol (especially later at night);
- Adrenal, liver, and/or hypothalamus insufficiency.
What triggers the hot flash? Theories:
Believe it or not, several studies have attempted to provoke hot flashes to better understand them. Brave women who want to make a difference for all of us found that:
- Most research suggests that hot flashes occur when decreased estrogen levels cause your body’s thermostat (hypothalamus) to become more sensitive to slight changes in body temperature. When the hypothalamus thinks your body is too warm, it starts a chain of events — a hot flash — to cool you down.
- Going from cool to a warm room triggers a hot flash in women who experience them but not in those who don’t.
- While starting new physical activity can bring on hot flashes, most likely by raising core temperature in an unacclimated body, habitual physical activity can lower their occurrence.
- Chemicals in the environment that mimic estrogen can increase apparent levels or block the very cell sites (receptors) where our native estrogen should dock and activate a cellular response. Blocking these receptors mimics a low estrogen condition even when labs show normal blood levels. These include:
- Phthalates- found in many personal care products especially perfumes, deodorants and lotions, plastics, shower curtains, children’s toys… are a large class of ubiquitous synthetic chemicals. Phthalates are also used in pesticides, wood finishes, adhesives, solvents, lubricants, and in medical devices including tubing, blood bags, surgical gloves, and dialysis equipment. Exposure can increase the risk of hot flashes. They also reduce the levels of testosterone.
- While PCBs are no longer used in manufacturing, this family of chemicals persist in the environment and can still be found in old electrical equipment. Depending on the specific form of PCB, they can either act like estrogen or block it.
- Plastics containing BPA and similar leach into the contents, especially bottled water that has sat in a warm warehouse and food microwaved in plastic or with plastic wrap.
- Organic, grass-fed, pasture raised meats and wild-caught (never farmed) fish are not given hormones to grow fatter faster, nor are they loaded up with toxic chemicals that mimic estrogen.
- Anxiety and/or depression can lead to increased hot flashes.
There are three major forms of estrogen:
- Estrone (E1) is the primary form made by adrenals and fat after menopause—this is further categorized into three main forms:
- 2-OH-E1 (considered protective from estrogen-linked cancers, is reduced by diets high in sugar, moderate to high alcohol consumption, while improved with cruciferous vegetables, fish oil and flax seeds).
- 4-OH-E1 (considered a dangerous form and causes genetic alterations. It is nearly double in women with breast cancer and may even be a biomarker—this form is made by a specific liver enzyme that, when elevated especially by smoking and other toxic exposures, will make estrogen precursors into this form).
- 16-OH-E1 (although weaker than 4-OH-E1 elevated levels also are linked with higher rates of breast cancer. That said, it is important for bone mineralization).
- Estradiol (E2) is the primary form of estrogen during reproductive years.
- Estriol (E3) is the primary form during pregnancy.
- Progesterone helps the uterus receive a fertilized egg and support the developing fetus. This function is irrelevant after childbearing years, but progesterone still needs balance with estrone although what that balance should be is a source of debate.
The problem is several-fold:
- At all phases of life, these hormones do not change at the same rate.
- In overweight women, adipose also produces quite a bit of estrone but not progesterone making those women estrogen dominant (which makes it very difficult to lose weight).
- Production of any of these can fluctuate. In other words, sometimes a perimenopausal woman can be estrogen dominant and sometimes progesterone dominant and then estrogen again, causing an average of 4-5 years mysterious symptoms.
Should we mess with hormone replacement treatments (HRT) or even hormone precursors like DHEA?
It is common for medical professionals to prescribe HRT for these reasons:
- The frequency and severity of symptoms associated with perimenopause and menopause;
- To bring hormones to childbearing levels—especially after a hysterectomy where the abrupt hormone changes are quite imbalanced; and/or
- To slow or even prevent osteopenia and osteoporosis.
The difference between “bioidentical” and synthetic. Derived primarily from various plants bioidentical is not exactly the same as the form made by us humans. Not identical but close. I have a lot of success with Wild Yam Complex, Black Cohosh, and certain adoptgens (adrenal gland balancing) by Mediherb; a blend of herbs used in clinical trials. I also always use Nutrition Response Testing to ensure it is a good fit—there are other options. Standard Process’ Wheat Germ Oil and Wheat Germ Oil Fortified provide nutrients to improve vaginal lubrication as examples.
Synthetic hormones are often derived from horses or made using other lab methods and are not the same at all as what is made by humans.
The transition through menopause has been occurring for eons. In contrast, HRT, a sedentary lifestyle, and Western diet of processed food and too much sugar are relatively recent—perhaps 80 years. We’re marketed heavily to buy these items and from such a very young age it changes how we think about food—”deprivation” no longer has something to do with what our bodies need to remain healthy, which sets us up for an uncomfortable menopausal transition among other health problems. I did an invited interview on the topic here.
The problem with using precursors is that they can be transformed into the dangerous forms of estrone (E1) if diet, lifestyle, certain medications… are favoring a liver pathway associated with producing the dangerous 4-OH version or relatively high levels of 16-OH.
In all cases, strive to take the lowest dose for the shortest amount of time to treat your menopausal concerns. This is true for most medications.
Options beyond HRT
While a personal choice, lifestyle habits, gut health issues, chronic stress experiences, environmental toxicant exposures, and blood sugar sensitivities are all important components to address.
My “go-to” list is:
- A food-based detoxification regimen to decrease the toxic load;
- Consistent diet and lifestyle changes including key whole foods that support a healthy gut environment; and
- Support for the hypothalamic-pituitary-adrenal (HPA).
These can be the “missing link” in the successful treatment of hormonal imbalances. Your liver has to do the balancing between hormones, among some 560 other things. That’s why a whole foods cleanse is often the first successful action.
Supplemental herbs and/or foods can shift the balance depending on which way we want it to go: Increase progesterone to align with estrogen dominance? Decrease testosterone? Make sure the form of estrogen is the healthy form, not dangerous—one of three main forms is more carcinogenic?
It really depends on each individual’s goals and philosophy, their health history, and past diet and lifestyle choices. Hormonal treatments don’t give the body a choice. HRT will sabotage the attempt by the body to try and manage this transition naturally. Not allowing the body to balance itself can worsen the symptoms listed earlier.
It’s good to know your hormone levels, or a good approximation, and how they cycle throughout the day including cortisol. Once a day is not enough as they fluctuate relative to each other throughout the day. Many practitioners look at only one time snapshot, Important to know the cycles: Morning, mid-day, afternoon, before bed at least. Cortisol is involved in both the stress response and plays a role in blood sugar levels that can trigger hot flashes. Postmenopausal serum estrogen (as estrone) should approach 50 pg/mL for bone strength. These numbers are different if measured by a blood spot or saliva (which shows the active level).
The test I like the best is Precision Analytical’s Dutch test: https://dutchtest.com/product/dutch-complete-2/ It is fairly costly and potentially can be covered by insurance if an ND, DO, or MD orders it. This test returns a robust report that shows you exactly what the body is doing throughout the day.
Nutrient and lifestyle-based strategies to balance hormones are the best initial choice. They are harmless and are easily available.
Start with the Standard Process 21-day purification program. It supports all the organs involved in balancing hormones and helps . It greatly helps the liver remove hormone-like toxic chemicals from the body and helps rebalance the gut microbiome. When you do this regimen with me as part of your Nutrition Response Testing program, you get daily guidance by email and we can tailor your individualized program with in-person Nutrition Response Testing visits.
A note of caution: There are a lot of blogs suggesting specific herbs. Please, before you decide to self-prescribe herbal remedies, please work with a professional who understands each and please only purchase the highest quality therapeutic grades. There is no better brand than Mediherb. For one, they require a professional license to make recommendations. Their quality control is amazing; unlike any other. Generally, different foods can be used to help balance hormones because they contain various compounds that either stimulate estrogen production or look like estrogen or block innate estrogen if a person happens to be estrogen dominant. Timing of carbohydrates can also help.
- Yams and flax seeds (organic) contain phytoestrogens (compounds that look like estrogens but come from plants rather than horses.
- Legumes: While soy is high in phytoestrogens, in the U.S. it is also mostly genetically modified to grow in Roundup which will increase toxic load. Even soy grown under organic conditions can cross with GMO versions. Better options include smaller beans such as mung beans, lentils, chickpeas, peas, and green beans. Red clover belongs to the legume family of plants. Sipping tea made from red clover may help but pregnant or breast feeding ladies should not use it.
- Certain fruits especially berries, dried plums (prunes) and apples.
- Vegetables like sprouts, cabbage, spinach, garlic, onion, and a compound in broccoli has been shown to improve estrogen status and reduce bone demineralization. Potatoes are also a good source of isoflavones.
- Foods high in resveratrol (an antioxidant) including grape skins, red wine, unsweetened grape juice, peanuts, cocoa, and certain berries including blueberries, bilberries, and cranberries can improve estrone quality by inhibiting the pathway to 4-OH-E1 and improving the protective pathway to 2-OH-E1. Resveratrol foods also help balance blood sugar, cholesterol profiles, and overall cardiovascular health.
- Get enough protein. Most don’t and we need more with aging. Protein helps regulate blood sugar, is a building block for all hormones, and prevents muscle loss. Yet the internet has so many recommendations and ways of calculating it as to make this confusing. In general 1-1.6 grams protein per kilogram of body weight is ideal. A 150 pound person is roughly 70 kg. Depending on exercise intensity, would want 70-122 g protein daily or 02.5 – 4.5 ounces, minimally. Another way of looking at this is as percent of calories: For a 2000 calorie diet, get at least 35 percent of those calories from protein. 1 gram of protein has 4 calories. Thus the ideal range for a 150 pound person is 280 – 500 calories from protein.
- Beverages including small amounts of red wine, certain teas especially green tea, horsetail, and rooibos. These teas also support a healthy gut microbiome.
- Licorice tea acts to balance cortisol levels. A cup of tea in the morning or more often can improve low cortisol AM fatigue and in some of us afternoon fatigue. Important! Do not use licorice if you have high blood pressure. I have a supplement that we can test with the component removed that causes blood pressure to go higher yet still has the adrenal balance function.
- Culinary herbs you likely have in you cupboard include fenugreek, pepper, parsley, oregano, sage, rosemary, thyme, mint, ginger, garlic.
- Manage stress: Because your stress response will alter all your steroid hormones, practice mindfulness and/or take actions like yoga, walks to look at pretty things, anything at all that puts you in a calm state.
- Sleep 8 hours: I know, this may be difficult if your cortisol and other hormones are imbalanced. It should be the goal.
And please, pretty please, cycle your carbs. During menopause and after, for a few days in a row go as low carb as possible, then can add some back in. Yams and any of the legumes and fruit would be carbs, as is alcohol. Having these or even a meal or alcohol later in the evening can make things worse.
Select References
- Avis, N. E., Levine, B. J., Danhauer, S., & Coeytaux, R. R. (2019). A pooled analysis of three studies of nonpharmacological interventions for menopausal hot flashes. Menopause (New York, N.Y.), 26(4), 350–356.
- Barnard N.D., Kahleova H, Holtz DN, et al (2023). A dietary intervention for vasomotor symptoms of menopause: a randomized, controlled trial. Menopause. 30(1):80-87.
- Canivenc-Lavier M.C., Bennetau-Pelissero C. (2023) Phytoestrogens and health effects. Nutrients; 15(2):317.
- Chen, L.R., Ko, N.Y., Chen, K.H. (2019). Isoflavone supplements for menopausal women: a systematic review. Nutrients. 2019;11(11):2649.
- Cramer, H., Lauche, R., Langhorst, J., & Dobos, G. (2012). Effectiveness of yoga for menopausal symptoms: a systematic review and meta-analysis of randomized controlled trials. Evidence-based complementary and alternative medicine : eCAM, 2012, 863905.
- Freedman R. R. (2001). Physiology of hot flashes. American journal of human biology : the official journal of the Human Biology Council, 13(4), 453–464.
- Gibson, C., Matthews, K., & Thurston, R. (2014). Daily physical activity and hot flashes in the Study of Women’s Health Across the Nation (SWAN) Flashes Study, 101(4), 1110-1116
- Gordon, J. L., Girdler, S. S., Meltzer-Brody, … Wisner, K. L. (2015). Ovarian hormone fluctuation, neurosteroids, and HPA axis dysregulation in perimenopausal depression: a novel heuristic model. The American journal of psychiatry, 172(3), 227–236.
- Malmir, H., Saneei, P., Larijani, B., & Esmaillzadeh, A. (2018). Adherence to Mediterranean diet in relation to bone mineral density and risk of fracture: a systematic review and meta-analysis of observational studies. European journal of nutrition, 57(6), 2147–2160.
- Miao, S., Yang, F., Wang, Y., Shao, C., Zava, D. T., Ding, Q., & Shi, Y. E. (2019). 4-Hydroxy estrogen metabolite, causing genomic instability by attenuating the function of spindle-assembly checkpoint, can serve as a biomarker for breast cancer. American journal of translational research, 11(8), 4992–5007.
- Slupski W, Jawien P, Nowak B. Botanicals in postmenopausal osteoporosis. Nutrients. 2021;13(5):1609.
- Thurston, R. C., Ewing, L. J., Low, C. A., Christie, A. J., & Levine, M. D. (2015). Behavioral weight loss for the management of menopausal hot flashes: a pilot study. Menopause (New York, N.Y.), 22(1), 59–65.
- Quattrini, S., Pampaloni, B., Gronchi, G., Giusti, F., Brandi, M. (2021) The Mediterranean diet in osteoporosis prevention: an insight in a peri- and post-menopausal population. Nutrients;13(2):531.
- Shah, B. R., Xu, W., & Mraz, J. (2019). Cytochrome P450 1B1: role in health and disease and effect of nutrition on its expression. RSC advances, 9(36), 21050–21062.
- Vrachnis, N., Zygouris, D., Vrachnis, D., … Iliodromiti, Z (2021). Effects of hormone therapy and flavonoids capable on reversal of menopausal immune senescence. Nutrients. 2021;13(7):2363.
- Ware W. R. (2009). Nutrition and the prevention and treatment of cancer: association of cytochrome P450 CYP1B1 with the role of fruit and fruit extracts. Integrative cancer therapies, 8(1), 22–28.
- Ziv-Gal, A., Gallicchio, L., Chiang, C., Ther, S. N., Miller, S. R … Flaws, J. A. (2016). Phthalate metabolite levels and menopausal hot flashes in midlife women. Reproductive toxicology (Elmsford, N.Y.), 60, 76–81


Leave a Reply
You must be logged in to post a comment.