If you have diabetes or even pre-diabetes (hypoglycemia), maintaining stable blood sugar throughout the day is vital. Depending on where you fall in the diabetes disease trajectory—and which form of diabetes you have—stabilizing blood sugar will be a combination of eating appropriate foods: starches and fruits, proteins, and fats; timing meals throughout the day; spreading carbs, proteins, and fats throughout the day; and potentially taking diabetes medications as directed by your doctor.
Whether or not you’ve progressed to needing diabetes medications, it’s important you keep your blood sugar under control. Let’s take a look how. Knowledge is Power.
Diabetes is not just about insulin and blood sugar
Although most of us understand that diabetes (both type 1 and type 2) is a failure of the body to keep blood sugar within a healthy range, few of us appreciate the complex web of interactions that control blood sugar; much less how to fix what’s wrong when blood sugar goes out of control.
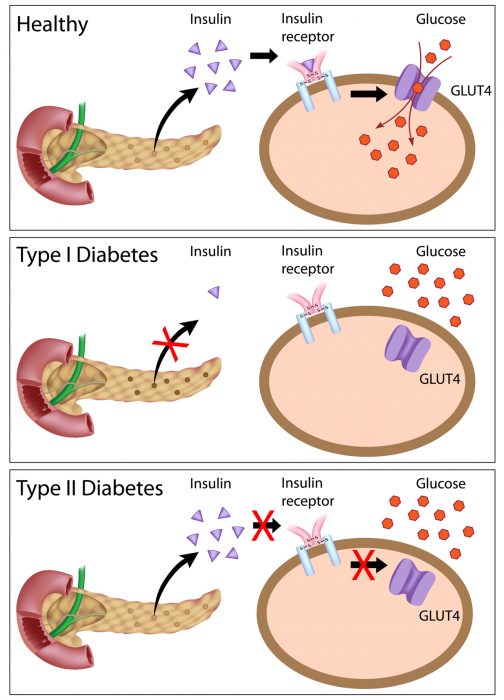
Despite sharing a name, type 1 and type 2 diabetes are quite different.
In type 1 diabetes: the body’s immune system has begun to attack the cells of the pancreas that produce insulin (beta cells). This autoimmune mistake limits the amount of insulin that can be produced. In fact, research has shown that there may be a 50 percent reduction in pancreatic beta cells before the disease is even diagnosed.
In type 2 diabetes: excess weight and inactivity change how liver, muscle (including smooth muscle of the digestive tract and other places, and cardiac muscle), adipose (fat), and even brain cells respond to insulin (Alzheimer’s may, in part, be linked to insulin resistance). At first, the pancreas can make plenty of insulin. That cola, or desert, elevates blood sugar and the pancreas responds by making more insulin to prevent blood sugar from going to high. The long-term trajectory—if blood sugar remains unaddressed—is pancreatic overload. Type 2 diabetics will also lose beta cell function.
While the pancreas is doing exactly what it is supposed to do, reducing blood sugar by stuffing more glucose into liver, muscle, and adipose cells doing so is not such a good idea. Regardless of the type of diabetes, glucose entering cells and then not immediately used for energy or to restore glycogen (only found in liver and muscle cells) is converted to fats (high blood triglycerides and weight gain). The cells experience substantial oxidative stress and begin to function poorly. Rather than succumb, the cells barricade the doors against more glucose entry. This is insulin resistance.
Using whole foods to reverse insulin resistance—key principles
The good news: Improving diet, managing stress, sleeping well, and other lifestyle changes can help stabilize blood sugar and improve insulin sensitivity in both types of diabetes. If recently diagnosed and only borderline indicators, type 2 diabetes can be completely reversed—and some people have used diet and lifestyle changes to reverse type 2 diabetes they’ve had for a long time.
Key Principle #1. First and foremost: A healthy eating plan for diabetes includes a mix of whole foods in the closest form possible to how they are found in nature. Skip the high saturated fat, high salt, added sugar, preservatives, food dyes, processed foods.
Key Principle #2. Eat portion sizes that help you achieve and maintain a healthy weight.
Key Principle #3. Spread your carbohydrates throughout the day and eat roughly the same amount of carbohydrates each day. Skipping meals may lead to low blood sugar.
Key Principle #4. There is no perfect nutrient ratio. While the American Diabetes Association (ADA) advocates 50 percent calories from carbohydrates, 30 percent calories from fats, and 20 percent calories from protein; you may feel your best using other ratios. For example, the macronutrients in the Paleo diet include high amounts of fat and much less carbohydrates. Several well-done studies indicate this approach works better than the ADA recommendations although it is not clear whether the difference is due to the macronutrient differences or the fact that Paleo-based recommendations tend to eliminate the worst inflammatory foods. See next.
Key Principle #5. Pay attention to food hypersensitivities. Eating foods that inflame your digestive tract, even a little, will increase immune system response. Especially in type 1 diabetes where the immune system is attacking the beta cells, we must work toward keeping inflammatory processes low and the immune system calm. Because one response to inflammation is elevating blood sugar, understanding and eliminating inflammatory foods is equally important.
Another reason a healthy digestive tract helps in diabetes
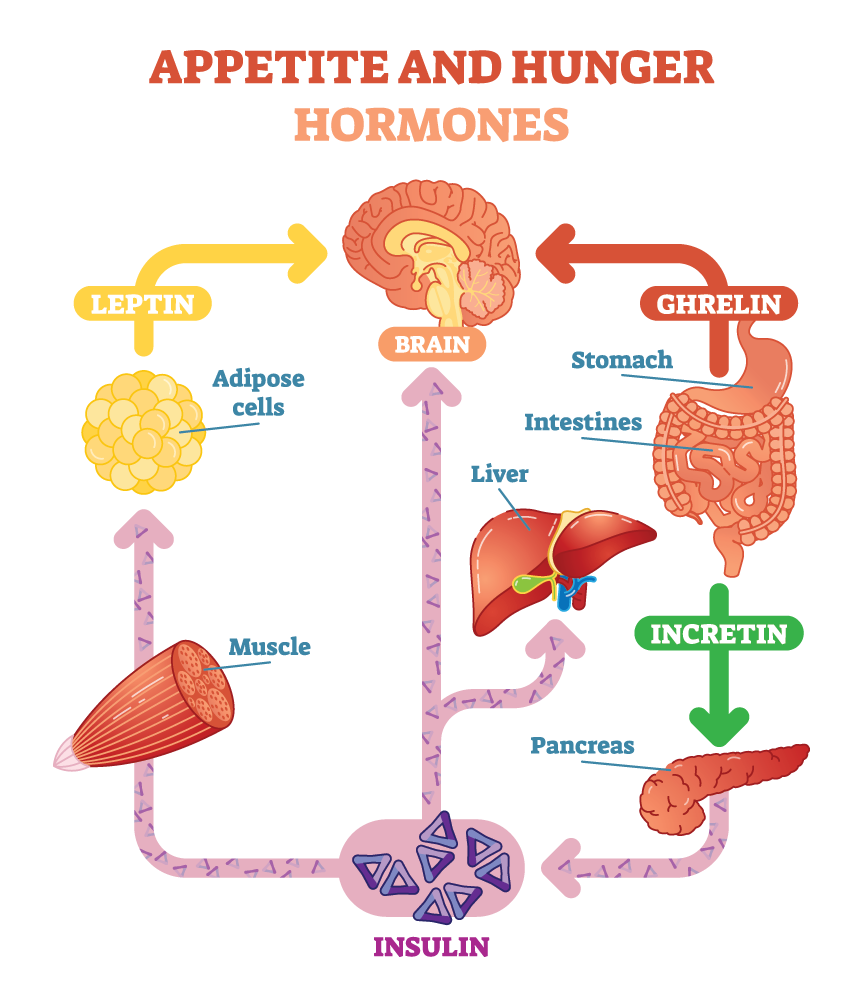 Cells in your gut make hormones involved in managing blood sugar called “incretins”. These special hormones are made minutes after eating a meal and do two key things:
Cells in your gut make hormones involved in managing blood sugar called “incretins”. These special hormones are made minutes after eating a meal and do two key things:
- Incretins control how much insulin is released by the pancreas, and
- Incretins improve insulin sensitivity.
Improving gut health improves the “blood sugar rollercoaster” even if beta cell function is compromised. And… in animal studies, improving the gut microbiome improves and balances immune function in a way the lessens autoimmune symptoms.
Putting it all together
Let’s say that 2000 calories is a good daily intake. For example, a diabetic wants to start with the ADA’s recommended 50/30/20 split of carbs, fats, protein.
Start with carbohydrates: half of 2000 calories equals 1000. Each gram of carbohydrates provides 4 calories, therefore daily grams of carbs is 250 grams. Looking at food labels or online databases (the best one is here and is FREE), tally up all the carbs in the foods you are eating. Whole foods high in starch include buckwheat, amaranth, millet, potatoes, wild rice, peas, winter squash, yams or sweet potatoes… (note: seeds from grass family plants are intentionally left off this list. Wheat, corn, rice, rye, oats, barley all have proteins in them that create gut inflammation and go against your health goals).
- Reality check #1: are you close to your target total carbohydrates?
- Reality check #2: are your carbs equally spaced throughout the day, including any snacks?
Work out your proteins: 20 percent of calories come from protein equals 400 calories. At 1 gram protein provides 4 calories, that’s 100 grams daily BUT each 15 grams of starchy whole foods will typically contain 3 grams of protein. Mathematically this works out to 50 grams protein already in the meal so our diabetic needs to find 50 more grams of protein from non-starchy sources: Fish, eggs, chicken, lean meats… or if vegetarian very large portions of non-starchy vegetables, especially spinach and other dark greens, asparagus, artichokes, brussels sprouts, and broccoli.
- Reality check #3: are you getting enough protein?
Then work out your fats: 30 percent of calories come from fat equals 600 calories. At 1 gram of fat provides 9 calories, allow for 67 grams daily. BUT some of your carb and protein choices contain fats, especially avocados, nuts, and animal/fish proteins—which is where it gets tricky and where a tool like this online app is a lifesaver.
- Reality check #4: are you using healthy fats? Fish, avocados, eggs, and olive oil provide some of the healthiest fats on the planet and are research-shown to improve blood sugar management.
Does this sound complicated? Your next visit we can complete my nutrients worksheet and I can even create customized meal plans.
Specific vitamins, minerals, and herbs help control blood sugar by improving insulin response and/or reducing autoimmune levels.
- Reality check #5: Depending on your individual situation you may benefit from specific herbs, minerals, or vitamins. BUT you will not benefit by trying spending money on supplements that won’t help your situation.
Let’s get you on the fast track to feeling good. I use Nutrition Response Testing to individualize supplements. No more guessing. Only specific herbs and nutrients help restore your organs.
There is hope and I can help: 907-222-1824
Arnold, S. E., Arvanitakis, Z., Macauley-Rambach, S. L., Koenig, A. M., Wang, H. Y., Ahima, R. S., … Nathan, D. M. (2018). Brain insulin resistance in type 2 diabetes and Alzheimer disease: concepts and conundrums. Nature reviews. Neurology, 14(3), 168–181.
Cicero L. T. Chang, Yenshou Lin, Arlene P. Bartolome, Yi-Ching Chen, Shao-Chih Chiu, and Wen-Chin Yang, (2013) Herbal Therapies for Type 2 Diabetes Mellitus: Chemistry, Biology, and Potential Application of Selected Plants and Compounds. Evidence-Based Complementary and Alternative Medicine, vol. 2013, Article ID 378657.
de Menezes, E., Sampaio, H., Carioca, A., Parente, N. A., Brito, F. O., Moreira, T., … Arruda, S. (2019). Influence of Paleolithic diet on anthropometric markers in chronic diseases: systematic review and meta-analysis. Nutrition journal, 18(1), 41. doi:10.1186/s12937-019-0457-z
Lim, E. L., Hollingsworth, K. G., Aribisala, B. S., Chen, M. J., Mathers, J. C., & Taylor, R. (2011). Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia, 54(10), 2506–2514.
Masharani, U., Sherchan, P., Schloetter, M., Stratford, S., Xiao, A., Sebastian, A., … Frassetto, L. (2015). Metabolic and physiologic effects from consuming a hunter-gatherer (Paleolithic)-type diet in type 2 diabetes. European Journal Of Clinical Nutrition, 69(8), 944–948.

Leave a Reply
You must be logged in to post a comment.